



















Vasectomy is a safe and effective method of permanent contraception and performed on approximately half a million men in the United
States every year. It is considered permanent although vasectomy reversal surgery can be performed to re-establish fertility.
Vasectomy
is still less preferred over tubal ligation despite being less expensive and associated with much less complications. Some men fear
pain while others equate vasectomy with castration or loss of masculinity. This is not true as vasectomy only disrupts the sperm flow
but testosterone hormone production of the testis which is responsible for normal male libido, erection and other masculine features.
Vasectomy
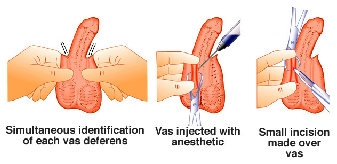
can be performed under local or general anesthesia as a day surgery in less than 40 minutes. Local anesthetic is usually given with
mild sedation to relax the patient and the scrotum. The vas is trapped between the surgeon’s fingers and local anesthetic is injected.
Studies in the United States, China and Thailand have shown that this technique results in significantly reduced incidence of swelling,
infection and pain, in addition to shorter surgical time. Although this method appears deceptively simple, it is more difficult to
learn than conventional vasectomy and should only be performed by urologists or practitioners who have been trained in this technique.
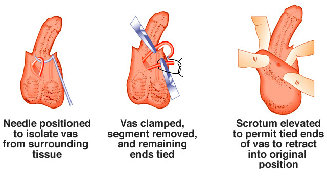
An alternative method called the ‘No-scalpel vasectomy’ or ‘Scalpeless vasectomy’ technique was developed and popularized in China
in 1974. It was introduced to the United States in 1985 and has since gained much popularity worldwide.
This technique eliminates
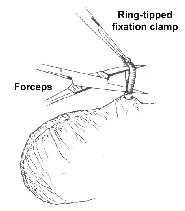
the use of the scalpel, results in a smaller wound than conventional vasectomy. The vas is mobilized to the skin and held in position
by a ring-tipped fixation clamp. A sharp, pointed, curve instrument (forceps) is used to puncture the skin and deliver the vas. The
rest of the procedure is similar to conventional vasectomy.
The patient can return to work almost immediately following vasectomy, as pain is minimal. Standard forms of contraception must still
be practiced till semen analysis at obtained at six weeks after the procedure to confirm absence of sperm. During this time, between
4-6 ejaculations are necessary to expel the remaining sperm. There is a 0.1% or less chance that the vas may recanalize and sperm
will re-appear in the semen.
After vasectomy, cells of the testes continue to produce testosterone hormone. Hence, blood testosterone
levels do not change after vasectomy and neither does the procedure induce early hypogonadism. The sperm-filled fluid from the testes
contributes about 10% to the volume of an ejaculation and does not significantly affect the appearance and texture of the ejaculate.
Sperm can no longer exit the body through the penis. They are broken down and absorbed by the body.
Minor swelling in the scrotum is the most common complication of vasectomy, with an average incidence of 2%. It is usually
minor and self-limiting. Sperm granulomas form when sperm leak from the testicular end of the vas and may sometimes cause chronic
post vasectomy pain. Chronic orchialgia or pain after vasectomy occurs only in 1 in 2000 patients.
There were recent studies
showing increased risk of prostate cancer in men who had a vasectomy. However, further studies and the National Institutes of Health
could not find a link between vasectomy and prostate cancer. The most likely explanation is detection bias. Vasectomized men are more
likely to visit an urologist and therefore, more likely to have cancer diagnosed earlier.

